Achilles Tendon Disorders
What is the Achilles Tendon?
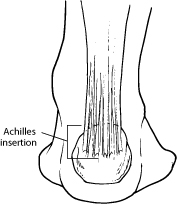
The Achilles tendon – where Achilles tendon disorders occur – is the band of tissue that runs down the back of the lower leg, connecting the calf muscle to the heel bone. Also called the heel cord, the Achilles tendon facilitates walking by helping to raise the heel off the ground.
Achilles Tendonitis and Achilles Tendonosis
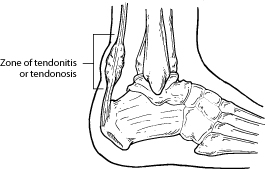
Two common disorders that occur in the heel cord are Achilles tendonitis and Achilles tendonosis.
Achilles tendonitis is an inflammation of the Achilles tendon. This inflammation is typically short-lived. Over time, if not resolved, the condition may progress to a degeneration of the tendon (Achilles tendonosis), in which the tendon loses its organized structure and is likely to develop microscopic tears. Sometimes the degeneration involves the site where the Achilles tendon attaches to the heel bone. In rare cases, chronic degeneration with or without pain may result in rupture of the tendon.
Causes of Achilles Tendon Disorders
As “overuse” disorders, Achilles tendonitis and tendonosis are usually caused by a sudden increase of a repetitive activity involving the Achilles tendon. Such activity puts too much stress on the tendon too quickly, leading to micro-injury of the tendon fibers. Due to this ongoing stress on the tendon, the body is unable to repair the injured tissue. The structure of the tendon is then altered, resulting in continued pain.
Athletes are at high risk for developing disorders of the Achilles tendon. Achilles tendonitis and tendonosis are also common in individuals whose work puts stress on their ankles and feet, such as laborers, as well as in “weekend warriors”—those who are less conditioned and participate in athletics only on weekends or infrequently.
In addition, people with excessive pronation (flattening of the arch) have a tendency to develop Achilles tendonitis and tendonosis due to the greater demands placed on the tendon when walking. If these individuals wear shoes without adequate stability, their overpronation could further aggravate the Achilles tendon.
Symptoms of Achilles Tendon Disorders
The symptoms associated with Achilles tendonitis and tendonosis include:
- Pain—aching, stiffness, soreness or tenderness—within the tendon. This may occur anywhere along the tendon’s path, beginning with the tendon’s attachment directly above the heel upward to the region just below the calf muscle. Pain often appears upon arising in the morning or after periods of rest, then improves somewhat with motion but later worsens with increased activity.
- Tenderness, or sometimes intense pain, when the sides of the tendon are squeezed. There is less tenderness, however, when pressing directly on the back of the tendon.
- When the disorder progresses to degeneration, the tendon may become enlarged and may develop nodules in the area where the tissue is damaged.
Diagnosis of Achilles Tendon Disorders
In diagnosing Achilles tendonitis or tendonosis, the surgeon will examine the patient’s foot and ankle and evaluate the range of motion and condition of the tendon. The extent of the condition can be further assessed with x-rays or other imaging modalities.
Treatment of Achilles Tendon Disorders
Treatment approaches for Achilles tendonitis or tendonosis are selected on the basis of how long the injury has been present and the degree of damage to the tendon. In the early stage, when there is sudden (acute) inflammation, one or more of the following options may be recommended:
- Immobilization. Immobilization may involve the use of a cast or removable walking boot to reduce forces through the Achilles tendon and promote healing.
- Ice. To reduce swelling due to inflammation, apply a bag of ice over a thin towel to the affected area for 20 minutes of each waking hour. Do not put ice directly against the skin.
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be helpful in reducing the pain and inflammation in the early stage of the condition.
- Orthotics. For those with overpronation or gait abnormalities, custom orthotic devices may be prescribed.
- Night splints. Night splints help to maintain a stretch in the Achilles tendon during sleep.
- Physical therapy. Physical therapy may include strengthening exercises, soft-tissue massage/mobilization, gait and running re-education, stretching and ultrasound therapy.
When is Surgery Needed?
If nonsurgical approaches fail to restore the tendon to its normal condition, surgery may be necessary. The foot and ankle surgeon will select the best procedure to repair the tendon, based on the extent of the injury, the patient’s age and activity level, and other factors.
Prevention
To prevent Achilles tendonitis or tendonosis from recurring after surgical or nonsurgical treatment, the foot and ankle surgeon may recommend strengthening and stretching of the calf muscles through daily exercises. Wearing proper shoes for the foot type and activity is also important in preventing recurrence of the condition.
Haglund’s Deformity
What Is Haglund’s Deformity?
Haglund’s deformity is a bony enlargement on the back of the heel. The soft tissue near the Achilles tendon becomes irritated when the bony enlargement rubs against shoes. This often leads to painful bursitis, which is an inflammation of the bursa (a fluid-filled sac between the tendon and bone).
Causes of Haglund’s Deformity
Haglund’s deformity is often called “pump bump” because the rigid backs of pump-style shoes can create pressure that aggravates the enlargement when walking. In fact, any shoes with a rigid back, such as ice skates, men’s dress shoes or women’s pumps, can cause this irritation.
To some extent, heredity plays a role in Haglund’s deformity. Inherited foot structures that can make one prone to developing this condition include:
- A high-arched foot
- A tight Achilles tendon
- A tendency to walk on the outside of the heel.
Symptoms of Haglund’s Deformity
Haglund’s deformity can occur in one or both feet. The symptoms include:
- A noticeable bump on the back of the heel
- Pain in the area where the Achilles tendon attaches to the heel
- Swelling in the back of the heel
- Redness near the inflamed tissue
Diagnosis of Haglund’s Deformity
After evaluating the patient’s symptoms, the foot and ankle surgeon will examine the foot. In addition, x-rays will be ordered to help the surgeon evaluate the structure of the heel bone.
Nonsurgical Treatment
Nonsurgical treatment of Haglund’s deformity is aimed at reducing the inflammation of the bursa. While these approaches can resolve the pain and inflammation, they will not shrink the bony protrusion. Nonsurgical treatment can include one or more of the following:
- Medication. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce the pain and inflammation. Ice. To reduce swelling, apply an ice pack to the inflamed area, placing a thin towel between the ice and the skin. Use ice for 20 minutes and then wait at least 40 minutes before icing again.
- Exercises. Stretching exercises help relieve tension from the Achilles tendon. These exercises are especially important for the patient who has a tight heel cord.
- Heel lifts. Patients with high arches may find that heel lifts placed inside the shoe decrease the pressure on the heel.
- Heel pads. Pads placed inside the shoe cushion the heel and may help reduce irritation when walking.
- Shoe modification. Backless or soft backed shoes help avoid or minimize irritation.
- Physical therapy. Physical therapy modalities, such as ultrasound, can help to reduce inflammation.
- Orthotic devices. Custom arch supports control the motion in the foot.
- Immobilization. In some cases, casting may be necessary.
When Is Surgery Needed?
If nonsurgical treatment fails to provide adequate pain relief, surgery may be needed. The foot and ankle surgeon will determine the procedure that is best suited to your case. It is important to follow the surgeon’s instructions for postsurgical care.
Prevention
To help prevent a recurrence of Haglund’s deformity:
- wear appropriate shoes; avoid shoes with a rigid heel back
- use arch supports or orthotic devices
- perform stretching exercises to prevent the Achilles tendon from tightening
- avoid running on hard surfaces and running uphill


“Nulla quis lorem ut libero malesuada feugiat. Proin eget tortor risus. Curabitur aliquet quam id dui posuere blandit. Donec sollicitudin molestie malesuada. Curabitur non nulla sit amet nisl tempus convallis quis ac lectus.”

“Lorem ipsum dolor sit amet, consectetur adipiscing elit. Cras ultricies ligula sed magna dictum porta. Curabitur arcu erat, accumsan id imperdiet et, porttitor at sem. Lorem ipsum dolor sit amet, consectetur adipiscing elit."

“Pellentesque in ipsum id orci porta dapibus. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Quisque velit nisi, pretium ut lacinia in, elementum id enim. Vivamus magna justo, lacinia eget consectetur sed at tellus."
Address
Phone
Office Hours
Mon-Tues 8:00am - 4:00pm
Wed 10:00am to 6:00pm
Thurs-Fri 8:00am - 4:00pm
Send a Message